The vagus nerve and its impact on inflammation
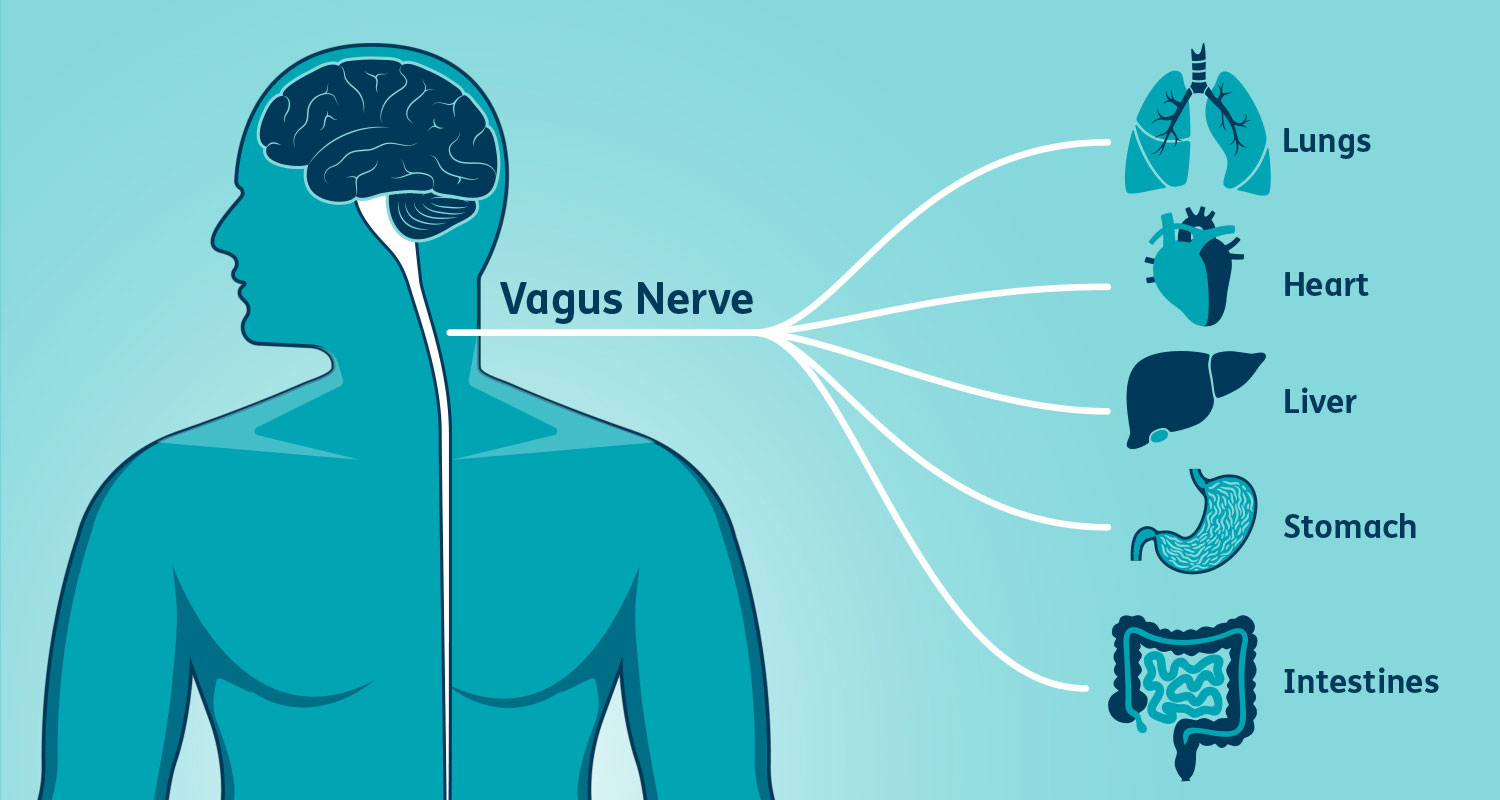
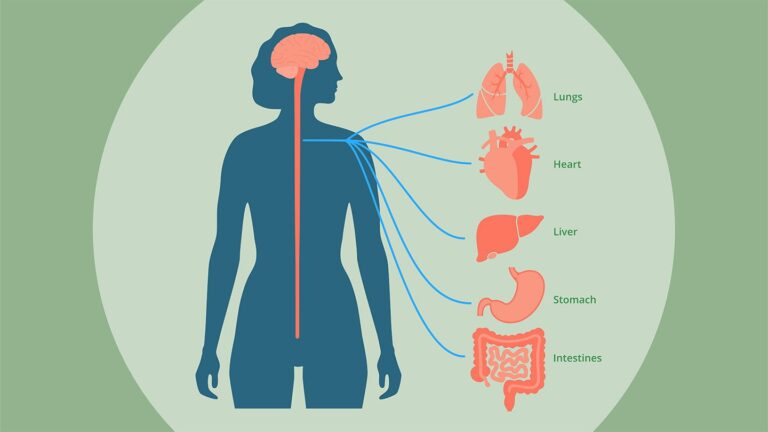
The vagus nerve, also known as the 10th cranial nerve, is a crucial component of the autonomic nervous system. It plays a significant role in regulating various bodily functions, including heart rate, digestion, and respiratory rate. However, recent research has highlighted another fascinating aspect of the vagus nerve: its role in inflammation.
Inflammation is a natural response of the body to protect itself from harmful stimuli, such as pathogens, irritants, or damaged cells. It is a complex process involving various immune cells, cytokines, and other signaling molecules. While acute inflammation is essential for healing and defense, chronic inflammation can lead to various health issues, including autoimmune disorders, cardiovascular diseases, and neurodegenerative diseases.
The vagus nerve exerts its anti-inflammatory effects through a pathway known as the cholinergic anti-inflammatory pathway. This pathway involves the release of acetylcholine, a neurotransmitter, by the vagus nerve. Acetylcholine then binds to alpha-7 nicotinic acetylcholine receptors on immune cells, such as macrophages and monocytes, inhibiting the production of pro-inflammatory cytokines, such as tumor necrosis factor-alpha (TNF-alpha) and interleukin-6 (IL-6).
Several studies have demonstrated the importance of the vagus nerve in modulating inflammation. For example, researchers have shown that electrical stimulation of the vagus nerve can reduce inflammation in animal models of sepsis, arthritis, and inflammatory bowel disease. Similarly, studies in humans have found that vagus nerve stimulation can improve symptoms in patients with autoimmune disorders, such as rheumatoid arthritis and Crohn’s disease.
Moreover, the vagus nerve’s role in inflammation extends beyond the immune system. Research has shown that vagus nerve stimulation can also modulate the activity of the hypothalamic-pituitary-adrenal (HPA) axis, a key regulator of the body’s stress response. By dampening the HPA axis’s activity, the vagus nerve can reduce the release of stress hormones, such as cortisol, which can exacerbate inflammation.
Interestingly, the gut microbiota, which plays a crucial role in immune function and inflammation, can also influence the vagus nerve. Studies have shown that the gut microbiota can communicate with the brain via the vagus nerve, a phenomenon known as the gut-brain axis. This communication can modulate the vagus nerve’s activity, thereby affecting inflammation and immune function.
Given the vagus nerve’s importance in regulating inflammation, researchers are exploring various ways to modulate its activity for therapeutic purposes. Vagus nerve stimulation, either through invasive techniques, such as surgically implanted devices, or non-invasive techniques, such as transcutaneous vagus nerve stimulation, is being investigated as a potential treatment for inflammatory disorders. Additionally, researchers are exploring the use of pharmacological agents that target the cholinergic anti-inflammatory pathway to reduce inflammation.
In conclusion, the vagus nerve plays a crucial role in modulating inflammation through the cholinergic anti-inflammatory pathway. By inhibiting the production of pro-inflammatory cytokines, the vagus nerve helps maintain immune homeostasis and prevent excessive inflammation. Understanding the vagus nerve’s role in inflammation could lead to new therapeutic strategies for treating inflammatory disorders and improving overall health.