Cervical Instability and Vagus Nerve-Related Symptoms
Cervical instability, characterized by abnormal movement of the cervical spine, has been associated with various symptoms that extend beyond localized neck pain. While the direct impact of cervical instability on the vagus nerve is not fully elucidated, emerging research suggests a potential interplay between cervical issues and the autonomic nervous system, wherein the vagus nerve plays a pivotal role. In this detailed article, we will explore the manifestations of cervical instability and its potential connection to symptoms related to the autonomic nervous system, focusing on the vagus nerve.
- Cervical Instability: An Overview:
Cervical instability refers to the abnormal movement of the cervical spine, often resulting from ligament laxity or damage. Common causes include trauma, degenerative changes, or congenital conditions. Symptoms of cervical instability encompass neck pain, stiffness, and a reduced range of motion, but recent investigations have expanded our understanding of its potential impact on broader physiological systems. - Symptoms of Cervical Instability:
Individuals with cervical instability may experience a spectrum of symptoms beyond localized neck discomfort. These symptoms include persistent neck pain, headaches, dizziness, vertigo, and even alterations in heart rate and respiratory function. Understanding these manifestations prompts exploration into the potential involvement of the autonomic nervous system. - The Autonomic Nervous System and Vagus Nerve:
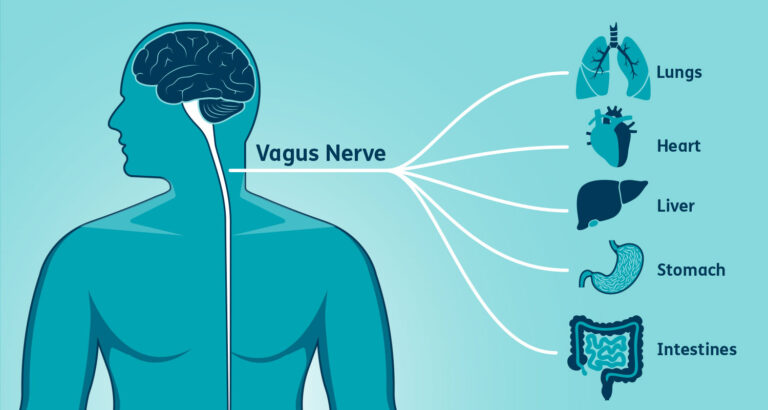
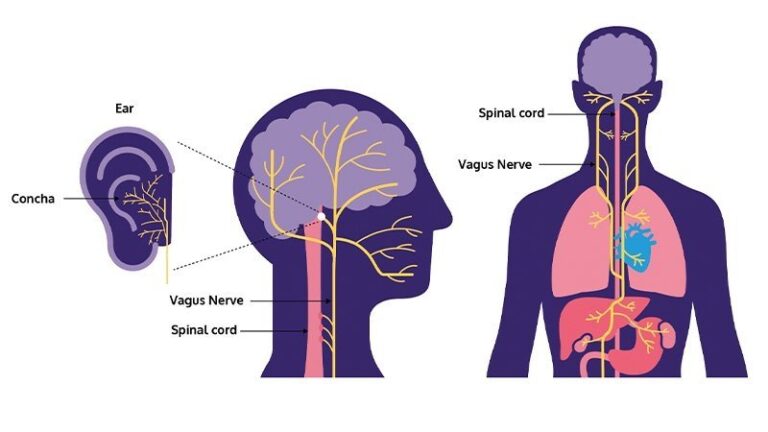
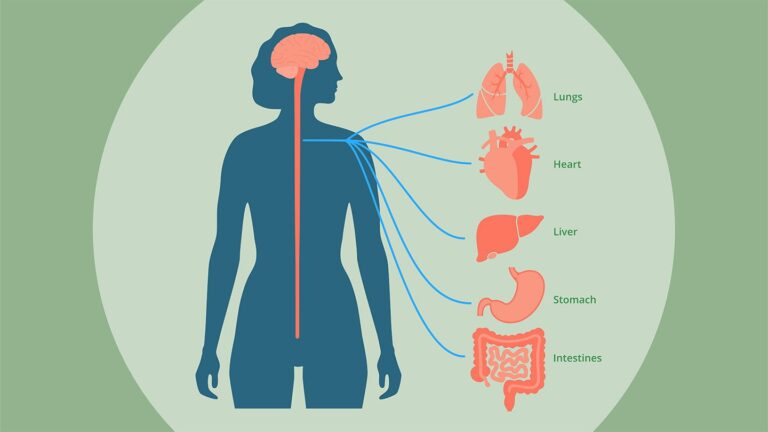
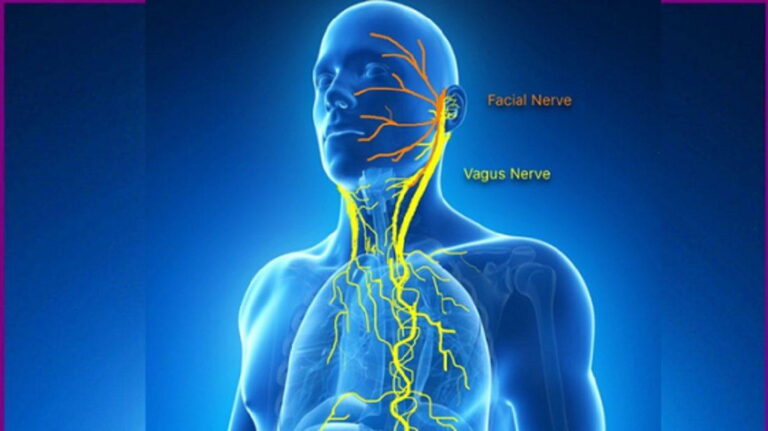
The autonomic nervous system regulates involuntary bodily functions, with the vagus nerve being a major component. It consists of two branches: the sympathetic and parasympathetic systems. The vagus nerve, part of the parasympathetic system, influences various vital functions, including heart rate, digestion, and respiratory rate. Disruptions in this delicate balance can lead to a range of symptoms affecting multiple organ systems. - Potential Connections Between Cervical Instability and Vagus Nerve Symptoms:
While research is ongoing, there is emerging evidence suggesting that cervical instability may indirectly influence the autonomic nervous system, potentially impacting vagus nerve function. Chronic neck pain and instability can contribute to increased sympathetic nervous system activity, affecting the balance between sympathetic and parasympathetic input. This dysregulation may manifest in symptoms such as irregular heart rate, dizziness, and gastrointestinal disturbances. - Clinical Considerations and Diagnosis:
Accurate diagnosis of cervical instability involves a comprehensive evaluation, including medical history, physical examinations, and imaging studies. Neurological assessments are crucial to identify potential vagus nerve-related symptoms. Collaboration between specialists such as neurologists, orthopedic surgeons, and physical therapists is often necessary for a multidisciplinary approach. - Treatment Approaches:
Treatment strategies for cervical instability vary based on the underlying cause and severity. Conservative approaches include physical therapy, pain management, and lifestyle modifications. In some cases, surgical interventions may be considered to address structural issues contributing to instability. Tailored treatment plans aim to alleviate symptoms and improve overall neck function. - Conclusion:
Cervical instability is a complex condition with implications that extend beyond localized neck pain. While the direct connection to vagus nerve symptoms is an area of ongoing research, understanding the potential interplay between cervical issues and the autonomic nervous system is crucial. Individuals experiencing symptoms related to cervical instability should seek professional medical evaluation to guide appropriate diagnosis and treatment, addressing both the structural aspects and potential autonomic implications for comprehensive care.